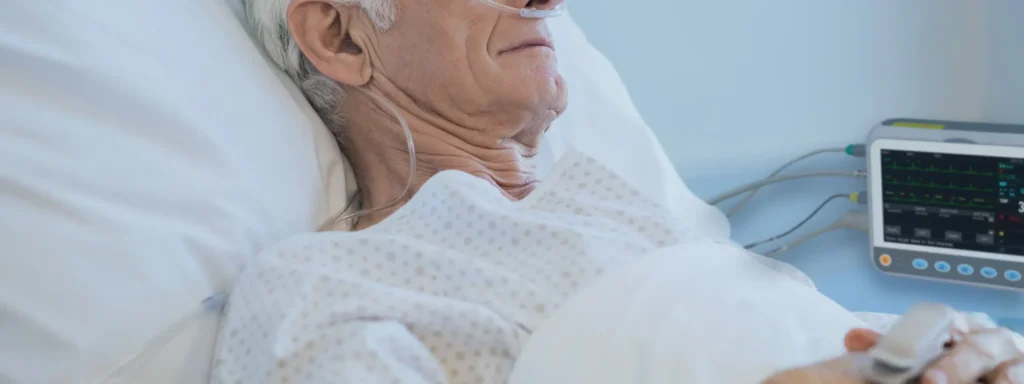
Obstructive Sleep Apnea Hypopnea Syndrome (OSAHS) is a common but often underdiagnosed condition that affects millions of adults worldwide. Characterized by repeated episodes of partial or complete obstruction of the upper airway during sleep, OSAHS can lead to a range of serious health issues, including cardiovascular disease, stroke, and daytime fatigue. Diagnosis of OSAHS is important, with traditional in-lab polysomnography considered the gold standard, but portable monitoring devices are changing how healthcare providers diagnose and treat the condition.
Understanding OSAHS and Its Impact on Health
Obstructive Sleep Apnea Hypopnea Syndrome (OSAHS) is characterized by intermittent airflow cessation in sleep because of the upper airway collapse or blockage. These interruptions, termed as apneas or hypopneas, might happen tens or hundreds of times throughout the night and will surely disrupt the normal pattern of sleep.
The symptoms usually seen with OSAHS include the following:
- Snoring
- Excessive daytime somnolence (strong tendency to fall asleep)
- Loud gasps or choking while asleep
- Headache on waking up
If left untreated, OSAHS can result in serious complications such as high blood pressure, heart disease, diabetes, and even stroke. Early diagnosis and intervention are critical to avoiding these long-term health risks.
Challenges in Traditional Diagnosis Methods
Traditionally, OSAHS has been diagnosed by polysomnography, which involves an overnight stay in a sleep laboratory with electrodes monitoring brain waves, muscle activity, heart rate, and airflow. Although valuable data is obtained with PSG, there are several disadvantages to this technique, including the following:
- Cost and Time: Testing in the lab can be costly, and patients may have to wait for weeks or even months for an appointment.
- Patient Discomfort: It is not always comfortable to stay in a sleep laboratory with wires attached to the body, and this may not be a reflection of normal sleep behavior.
- Accessibility: Sleep laboratories are not easy to access, especially in rural or remote areas; thus, many patients do not get timely diagnosis due to such unavailability.
For these reasons, portable monitoring devices have emerged as a game-changing solution for diagnosing OSAHS, allowing for a more convenient and accessible approach.
Portable Monitoring Devices: A Convenient Solution for OSAHS Diagnosis
Portable monitoring devices, otherwise known as home sleep apnea tests, are designed to monitor key physiological parameters associated with OSAHS in the comfort of a patient’s home. These devices have revolutionized sleep medicine by offering a less invasive, more affordable, and more accessible means of diagnosing adult OSAHS.
Key Features of Portable Monitoring Devices
Portable monitoring devices typically measure the following physiological parameters:
- Airflow: It involves the monitoring of breathing patterns through nasal cannulas or thermistors to detect apneas or hypopneas.
- Pulse Oximetry: This measures oxygen saturation in the blood, which is reduced during apneas.
- Heart Rate: Heart rates are monitored because during an apnea, heart rate increases due to the deprivation of oxygen.
- Respiratory Effort: It monitors chest movements to determine respiratory effort during sleep.
- Body Position: Monitors the patient’s position to determine if apnea events are positional, in that they occur more often when the patient is lying on their back.
By observing these parameters, portable monitoring devices are able to ascertain the frequency and severity of apneas and hypopneas and provide a very clear picture of whether a patient is suffering from OSAHS.

How Portable Monitoring Devices Address Diagnostic Needs
Ease and Comfort
Unlike in-lab testing, portable monitoring devices have the advantage of being conducted within the comfort of a patient’s home, minimizing disruption to the normal sleep pattern. Ease of use is also an important advantage for patients who may feel uncomfortable or anxious when staying overnight in a sleep lab. This approach at home lets one be more natural during sleep, hence data obtained would be reflective of the patient’s usual sleep behavior.
Cost-Effective and Accessible
Portable monitoring devices are relatively inexpensive compared to the traditional in-lab sleep tests, making OSAHS diagnosis a reality for more patients. This is very important for rural or underserved populations in which traveling to a sleep lab is a significant logistical burden. The portable monitors are also used in follow-up, monitoring treatment efficacy and potentially reducing the need for in-lab visits.
Prompt Diagnosis
The ability to perform the test at home allows the patient to undergo diagnosis for OSAHS without waiting. Providers can review the data after completion of the test and immediately start treatment recommendations. Diagnosis and timely intervention play an important role in managing the disease of OSAHS and preventing complications related to cardiovascular disease and diabetes.
Accurate Results
Many home sleep tests now offer comparable results to traditional in-lab polysomnography. While portable monitors may not have the same level of detail as full PSG, they still provide essential data for diagnosing moderate to severe cases of OSAHS. For patients with mild OSAHS or those who present with higher-risk profiles, these devices can still deliver accurate information that guides clinical decisions.

What Happens After Diagnosis?
Once a diagnosis of OSAHS is confirmed through portable monitoring, healthcare providers can recommend appropriate treatment options based on the severity of the condition. Common treatments include:
- Continuous Positive Airway Pressure (CPAP): A CPAP machine uses a steady stream of air to keep the airway open during sleep.
- Oral Appliances: These devices reposition the jaw to maintain an open airway.
- Lifestyle changes include weight loss, changing sleep posture, and avoiding alcohol intake before bedtime.
- Surgical Interventions: Severe cases are treated with surgery, where excess tissue or correction of structural problems in the airway is performed.
This allows healthcare professionals to use portable monitoring devices in order to track the treatment outcome and modify therapies as appropriate for each patient.
Conclusion: The Future of OSAHS Diagnosis with Portable Monitoring Devices
The use of portable monitoring devices in the diagnosis of adult OSAHS has increased accessibility, comfort for the patient, cost-effectiveness, and timeliness of diagnosis. These devices offer a practical and efficient solution for both patients and healthcare providers, overcoming many of the limitations associated with traditional in-lab testing. Portable monitors help in the identification of more cases of OSAHS and allow for earlier interventions, thus reducing the long-term risks associated with untreated sleep apnea, by their ability to deliver accurate results and provide valuable data.